A science‑led story about how non‑invasive brain stimulation compares with (and complements) mindfulness and meditation, from Tibetan Buddhist monks to modern fMRI and EEG labs.
On a Tuesday that felt suspiciously like a Monday in disguise, Ava realised her brain had the attention span of a golden retriever in a tennis‑ball factory. Slack pinged. News alerts flashed. Her coffee (third of the day) had a personality. By bedtime, the lights were out but her mind was still holding a staff meeting. If any of this sounds familiar, welcome — you’re living in the standard model of modern life.

Ava tried what many of us try: short mindfulness meditations between meetings, a longer practice on weekends, a blue‑light filter that made her laptop look like it was wearing sepia sunglasses. It helped… some. Then her coach mentioned Transcranial Magnetic Stimulation (TMS); not as a replacement for meditation, but as a circuit‑level nudge that might help her mind find the “off” switch again. That idea, practice from the inside out, and stimulation from the outside in, is the heart of this story.
What TMS actually is (and why it matters)
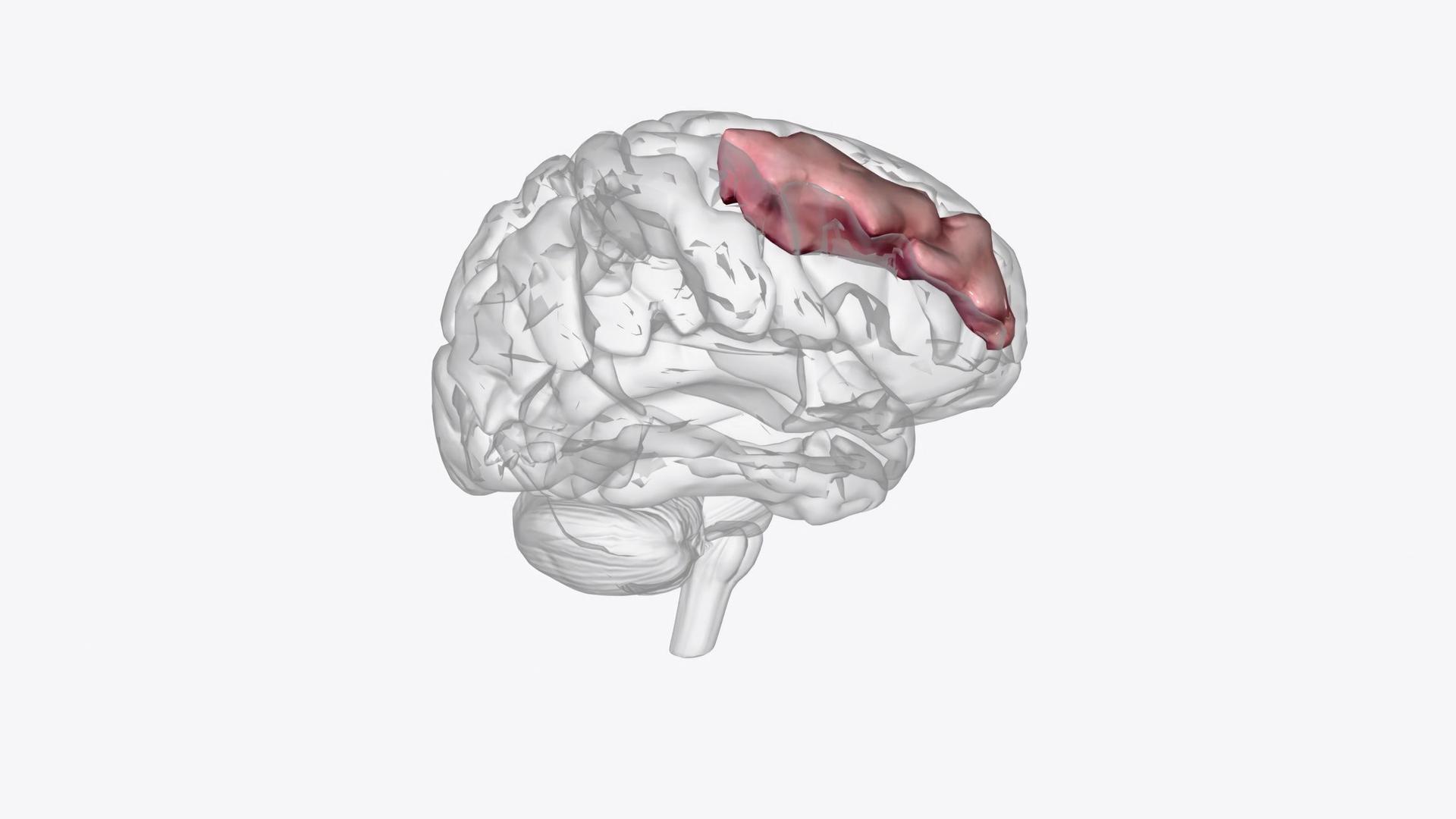
Here’s the elevator pitch: a small coil on the scalp sends magnetic pulses that induce tiny currents in the brain’s surface networks. The usual target is the dorsolateral prefrontal cortex — a bossy bit of cortex that helps with focus, mood regulation, and decision‑making (the inner adult who reminds you to go to bed). Sessions are done awake, there’s no anaesthesia, and side effects are typically mild. People often describe the sensation as rhythmic tapping. Think “neural metronome,” not “jumper cables.”
Over nearly forty years, TMS has moved from research rooms to everyday clinics. Protocols became shorter (theta‑burst formats), coil designs improved (some targeting is deeper, some more focal), and safety guidelines matured with millions of delivered sessions. Under those guidelines, the risk profile is favourable; the rarest concern, seizure, remains very low with proper screening and dosing. Translation: it’s a careful tool, not a blunt instrument.
Meanwhile, in the meditation hall (and lab)
Picture a quiet temple in the highlands. A Tibetan Buddhist monk sits perfectly still, breathing like the tide. In labs from Boston to Lyon, scientists noticed that experienced practitioners show changes you can measure: thicker cortex in attention hubs, increased grey matter in learning and memory regions after just eight weeks of mindfulness training, and calmer baseline activity in the Default Mode Network (the mental channel that plays reruns when you’re trying to sleep). EEG studies even found that monks trained in compassion practices can produce sustained, synchronized gamma‑band rhythms — the brain’s way of saying, “Everything’s clicking.”

Neurochemistry adds colour, though it’s trickier to pin down. Some studies show boosts in GABA (an inhibitory, calming neurotransmitter) after movement‑based practices like yoga; evidence is more mixed for seated mindfulness alone. PET work has observed dopamine shifts during deep meditation. If that sounds technical, just remember the everyday version: seasoned meditators often report steadier moods, less reactivity, and an easier time putting thoughts down at night; the subjective mirror of those objective findings.
(Jargon translator: DMN = your brain’s screensaver; gamma = high‑performance group chat for neurons; GABA = the brain’s mellow button.)
The comparison that actually matters
Meditation is like learning the piano: scales, drills, then music. Changes accrue with practice. TMS is like a tuning fork held to the instrument: it doesn’t write the melody, but it helps the strings settle into the right key so practice sounds better sooner. Both approaches converge on similar networks — prefrontal control systems, salience hubs that decide what’s important, and limbic regions that can overreact under stress. It’s little wonder the two pair well in the real world.

Ava did four weeks of structured practice with brief, daily meditations and sleep hygiene, alongside a TMS course designed to re‑engage those prefrontal circuits. The first thing she noticed wasn’t fireworks; it was subtle: the 2 a.m. spiral became a wobble, then a pause, then… silence. (Scientific term: “blissful nothing.”) Her coach tracked changes the boring but honest way: validated mood scales, sleep‑onset latency (time to fall asleep), and simple focus measures. Over time, the metrics lined up with how she felt.
What TMS treats and how it evolved
TMS built its reputation treating major depressive disorder, gaining the first U.S. FDA clearance back in 2008. Since then, specific devices and protocols have earned clearances for obsessive–compulsive disorder, smoking cessation, and aspects of migraine care. In parallel, session formats evolved from long, daily appointments to compact theta‑burst sessions measured in minutes. Throughout, iterative safety statements — informed by large datasets — refined who should and shouldn’t receive stimulation (for example, certain implants or epilepsy history call for caution or exclusion). The net effect is a technology that’s more precise, quicker, and easier to live with.
Modern TMS for Wellness
Enter ExoMind by BTL — a modern TMS platform that is FDA‑cleared for depression and increasingly used in wellness‑aligned programmes focused on emotional regulation, cognitive clarity, and sleep support. ExoMind’s approach to targeting (ExoTMS®) emphasises the same mood‑relevant networks studied in traditional rTMS, packaged in a calmer, more accessible session experience. In wellness contexts, it sits alongside coaching, mindfulness, and sleep routines; the point isn’t to replace practice, but to help it stick. (Think: fewer heroic willpower moments, more “this is just how my brain works now.”)

Safety first: Even in wellness programmes, TMS requires proper screening and clinician oversight. Individual responses vary, and any existing diagnoses or medications should be coordinated with your healthcare provider.
The scientist’s aside (a tiny detour you can skip)
If you enjoy acronyms: mindfulness practice is associated with reduced amygdala reactivity and improved prefrontal–limbic coupling on fMRI, while TMS modulates excitability and connectivity in overlapping networks, sometimes producing downstream changes in cortisol, sleep architecture, and mood. If you don’t enjoy acronyms: meditation calms the alarm system; TMS helps the brakes work better. Done.
Putting it together
Ava didn’t become a monk (she still loves good espresso), and she didn’t outsource her mind to a machine. She combined daily, doable practice with a time‑limited TMS course. The music metaphor fits: meditation gave her the notes; TMS helped tune the instrument; life supplied the song. For the overstimulated, under‑slept, over‑caffeinated many, that pairing offers a realistic, evidence‑based path back to clarity and calm — with modern systems like ExoMind making the journey more accessible than ever.
If you're wondering how TMS or other mental health services might be able to help you, you can chat with experts and get immediate personalised suggestions on the MeTime app.







